Diabetes during pregnancy: What mothers must know
Manage diabetes during pregnancy smartly, Dr Uma Mishra explains here regarding risks and remedies when women have diabetes in pregnancy. Dr Uma Mishra is a leading gynecologist in Noida.
Dr Uma Mishra, MD
2/25/20243 min read

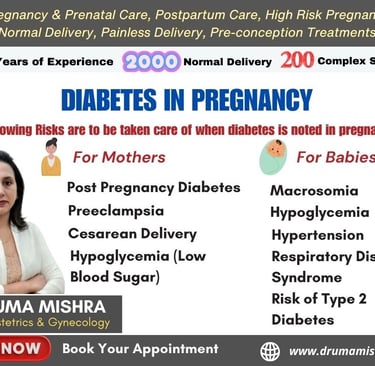
Diabetes during pregnancy, known as gestational diabetes, poses certain risks to both the mother and the baby. Dr Uma Mishra, one of the best Gynecologists in India explains some associated risks and recommendations for monitoring:
Risks for Mother:
Increased Risk of Type 2 Diabetes: Women with gestational diabetes have a higher risk of developing type 2 diabetes later in life.
Preeclampsia: There's an elevated risk of developing high blood pressure and preeclampsia.
Cesarean Delivery: There's an increased likelihood of needing a cesarean section.
Hypoglycemia (Low Blood Sugar): Sometimes, medications to control gestational diabetes can lead to low blood sugar levels.
Risks for Baby:
Macrosomia: Babies born to mothers with gestational diabetes may be larger than usual, leading to complications during delivery.
Hypoglycemia: The baby may experience low blood sugar levels after birth.
Respiratory Distress Syndrome: An increased risk of respiratory problems for the baby.
Risk of Type 2 Diabetes: Babies born to mothers with gestational diabetes may have a higher risk of developing type 2 diabetes later in life.
Monitoring and Care:
Increased Gynecologist Visits: The frequency of visits to the gynecologist will depend on the severity of the gestational diabetes and the individual case. Generally, more frequent check-ups are needed to monitor both the mother and the baby.
Blood Sugar Monitoring: Regular monitoring of blood sugar levels is crucial. This often involves self-monitoring at home with a glucometer and periodic lab tests. I am explaining here how expecting mother can do sugar monitoring during pregnancy:
A. Obtain a Glucose Meter:
Consult with your healthcare provider to determine the most suitable glucose meter for your needs.
Ensure the glucose meter is calibrated and in good working condition.
B. Gather Supplies:
Purchase test strips compatible with your glucose meter.
Ensure you have a lancing device to obtain a small blood sample.
Use alcohol wipes to clean the testing area.
C. Wash Hands:
Wash your hands thoroughly with soap and water. Avoid using hand sanitizer, as it may contain substances that can interfere with the readings.
D. Prepare the Lancing Device:
Load the lancet into the lancing device according to the manufacturer's instructions.
Adjust the depth setting on the lancing device based on your healthcare provider's recommendation.
E. Prepare the Glucose Meter:
Insert a test strip into the meter as directed by the manufacturer.
Ensure the meter is turned on and ready for testing.
F. Lance the Finger:
Choose a finger (usually the sides) for blood collection.
Use the lancing device to prick the side of your finger.
Allow a small drop of blood to form.
G. Apply Blood to Test Strip:
Touch the drop of blood to the designated area on the test strip.
Ensure that an adequate amount of blood is applied to obtain an accurate reading.
H. Wait for Results:
The glucose meter will display your blood sugar level after a few seconds.
Record the result in a logbook or on a digital device as recommended by your healthcare provider.
I. Interpret Results:
Understand the target blood sugar levels provided by your healthcare provider.
Be aware of the acceptable range for fasting and post-meal readings.
J. Follow Healthcare Provider Recommendations:
Share your blood sugar records with your healthcare provider during regular check-ups.
Follow any adjustments to your diet, exercise, or medication regimen as advised.
K. Maintain Regular Monitoring:
Monitor blood sugar levels as recommended by your healthcare provider. This may include fasting levels in the morning and post-meal levels after each main meal.
L. Seek Immediate Assistance:
Contact your healthcare provider if you experience consistently high or low blood sugar levels, or if you have concerns about your pregnancy.
Always consult with your healthcare provider for personalized advice and guidance on blood sugar monitoring during pregnancy. They can provide specific instructions based on your individual health condition and the requirements of your pregnancy.
Other important points for care for diabetic pregnant women are as follows:
Dietary Management: A carefully planned and monitored diet is essential. A Gynecologist can help create a suitable meal plan. Dr Uma Mishra, Gynecologist can help you manage through dietary plans during pregnancy.
Medication if Necessary: Insulin or other medications may be prescribed to control blood sugar levels. Regular medication management and adjustments may be needed. Your Gynecologist will assess your case and history and provide the required medication with suitable dose, if required.
Fetal Monitoring: Depending on the severity of the condition, fetal monitoring through ultrasounds and other tests may be recommended to check the baby's growth and well-being.
Blood Pressure Monitoring: Due to the increased risk of preeclampsia, blood pressure should be regularly monitored.
Regular Physical Activity: As recommended by the healthcare provider, maintaining regular physical activity can help manage blood sugar levels.
It's important to note that the management plan will be individualized based on the specific circumstances of each pregnancy. Women with gestational diabetes should work closely with their healthcare team to ensure proper monitoring and management throughout the pregnancy.
Dr Uma Mishra, Gynecologist is MD, Obs & Gyne and is one of the leading Gynecologists in India. You can book consultation at 8130550269.